Corneal Transplants
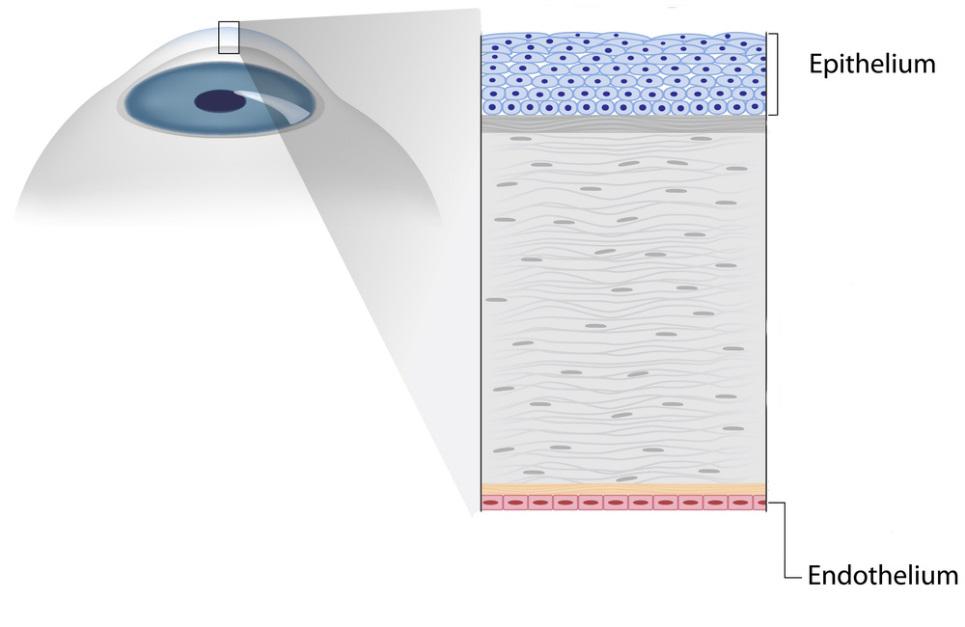
The cornea is the clear front window of the eye. The front surface is covered by a layer of skin called the epithelium. The back surface is covered by a layer of cells called the endothelium.
Many problems of the cornea can be treated medically, but in situations where the cornea cannot be healed or repaired adequately, surgical intervention may be required.
A corneal transplant is a surgery where your diseased cornea is replaced with the healthy cornea from a human donor. Donors are people who choose to donate their corneas after their death to patients who need this tissue. All donated corneas are carefully screened and thoroughly tested to make sure that they are healthy and safe to use. Corneal transplants are most commonly performed for corneal scars, Fuchs corneal dystrophy, and keratoconus.
Before proceeding with corneal transplant surgery, you should understand the risks of this procedure. These include (but are not limited to) bleeding, infection, increased eye pressure, vision disturbances (such as glare, halos around lights, and starbursts), inflammation of the retina, failure of the corneal transplant, rejection of the corneal transplant, chronic inflammation, double vision, droopy eyelid, retinal detachment, need for additional surgery or laser procedures, need for glasses or contact lenses, loss of vision, loss of the eye, and problems with anesthesia.
Generally speaking, there are two types of corneal transplants:
 A traditional full-thickness corneal transplant (or penetrating keratoplasty [PKP]) consists of removing all layers of the patient’s cornea and replacing them with a full-thickness donor cornea. A traditional full-thickness corneal transplant is the treatment of choice for corneal scars and other issues affecting the middle layers of the cornea. It is an effective procedure, and often it is the only procedure that can be used to fix a problem. Unfortunately, penetrating keratoplasty is also quite invasive with many drawbacks. It is a long surgery with high risks, recovery often takes more than 18 months, the best vision following recovery usually requires the use of a rigid contact lens, and there is a reasonably high chance of tissue rejection or failure.
A traditional full-thickness corneal transplant (or penetrating keratoplasty [PKP]) consists of removing all layers of the patient’s cornea and replacing them with a full-thickness donor cornea. A traditional full-thickness corneal transplant is the treatment of choice for corneal scars and other issues affecting the middle layers of the cornea. It is an effective procedure, and often it is the only procedure that can be used to fix a problem. Unfortunately, penetrating keratoplasty is also quite invasive with many drawbacks. It is a long surgery with high risks, recovery often takes more than 18 months, the best vision following recovery usually requires the use of a rigid contact lens, and there is a reasonably high chance of tissue rejection or failure.
 For patients with a problem that affects only the endothelial cells, a partial-thickness corneal transplant (or Descemet’s stripping endothelial keratoplasty [DSEK]) can instead be performed. This transplant consists of removing only the endothelial layer of the patient’s cornea and replacing it with only the endothelial layer of the donor cornea. A DSEK partial-thickness corneal transplant is the treatment of choice for issues affecting the backside of the cornea, such as Fuchs corneal dystrophy. Compared to penetrating keratoplasty, this newer procedure has multiple advantages. It is a shorter surgery, it is a safer surgery, recovery typically takes only 4 months, best vision following recovery does not require the use of a rigid contact lens, and the chances of rejection are much lower. Unfortunately, however, this type of transplant can only be performed in select cases for particular diseases.
For patients with a problem that affects only the endothelial cells, a partial-thickness corneal transplant (or Descemet’s stripping endothelial keratoplasty [DSEK]) can instead be performed. This transplant consists of removing only the endothelial layer of the patient’s cornea and replacing it with only the endothelial layer of the donor cornea. A DSEK partial-thickness corneal transplant is the treatment of choice for issues affecting the backside of the cornea, such as Fuchs corneal dystrophy. Compared to penetrating keratoplasty, this newer procedure has multiple advantages. It is a shorter surgery, it is a safer surgery, recovery typically takes only 4 months, best vision following recovery does not require the use of a rigid contact lens, and the chances of rejection are much lower. Unfortunately, however, this type of transplant can only be performed in select cases for particular diseases.
Both types of corneal transplants are performed on an outpatient basis, and you will get to go home the same day. At New England Vision, surgery is almost always done on the first floor in The Eye Surgery Center.
When you arrive for surgery, you will be given various eye drops, and an I.V. will be placed in your arm. For a full-thickness PKP, you may be put completely to sleep for your surgery. In contrast, for a partial-thickness DSEK, you will be awake for surgery, but relaxing medicine through your I.V. and numbing medicine near your eye will help you to stay calm and comfortable throughout the procedure.
In the operating room, the appropriate part of your diseased cornea is removed. For a penetrating keratoplasty, an instrument called a trephine is used to cut a precise round hole through the entire thickness of your cornea. The donor cornea is then cut to a matching size and carefully sewn into position using approximately 16 stitches.
For a Descemet’s stripping endothelial keratoplasty, the endothelial layer alone is stripped from the backside of the cornea and removed from the eye. The donor endothelium is then cut to a matching size, folded, and inserted into the eye. The graft unfolds inside of the eye, and after it is positioned correctly, it is secured in place using a bubble of air. With a DSEK, no stitches are used to keep the transplanted tissue in the proper position.
Regardless of the type of corneal transplant that you undergo, when surgery is over, you will have a bandage over your eye. With a PKP, there are no positioning requirements following surgery. However, with a DSEK, it is important to lie flat on your back for the first 24 hours after surgery. This allows the air bubble inside of the eye to maintain pressure against the back of the cornea and pin the new donor tissue into place.
All patients are seen in the office the next day for a post-operative appointment. Your doctor will discuss your activity restrictions, and he will review your postoperative eye drops. With a full-thickness transplant, healing then continues for over a year. There are multiple office visits throughout that time, and stitches are sequentially removed. With a partial-thickness transplant, healing often takes only 4 months. However, you will still be seen in the office regularly during that time to ensure that your eye is progressing appropriately. For both types of surgery, follow-up care is a key part of your treatment and safety. It is critical that you attend all scheduled appointments, and that you call your doctor if you are having any problems.
After your eye has fully recovered, your vision will likely be much better. However, it may never be perfect. Glasses (or for patients who get a PKP, rigid contact lenses) often help significantly, but they probably will still not be able to completely clear your vision. Improvement, and not perfection, is the goal of corneal transplant surgery.
Visit the American Academy of Ophthalmology’s EyeSmart® website to learn more about Corneal Transplants.
 A traditional full-thickness corneal transplant (or penetrating keratoplasty [PKP]) consists of removing all layers of the patient’s cornea and replacing them with a full-thickness donor cornea. A traditional full-thickness corneal transplant is the treatment of choice for corneal scars and other issues affecting the middle layers of the cornea. It is an effective procedure, and often it is the only procedure that can be used to fix a problem. Unfortunately, penetrating keratoplasty is also quite invasive with many drawbacks. It is a long surgery with high risks, recovery often takes more than 18 months, the best vision following recovery usually requires the use of a rigid contact lens, and there is a reasonably high chance of tissue rejection or failure.
A traditional full-thickness corneal transplant (or penetrating keratoplasty [PKP]) consists of removing all layers of the patient’s cornea and replacing them with a full-thickness donor cornea. A traditional full-thickness corneal transplant is the treatment of choice for corneal scars and other issues affecting the middle layers of the cornea. It is an effective procedure, and often it is the only procedure that can be used to fix a problem. Unfortunately, penetrating keratoplasty is also quite invasive with many drawbacks. It is a long surgery with high risks, recovery often takes more than 18 months, the best vision following recovery usually requires the use of a rigid contact lens, and there is a reasonably high chance of tissue rejection or failure. For patients with a problem that affects only the endothelial cells, a partial-thickness corneal transplant (or Descemet’s stripping endothelial keratoplasty [DSEK]) can instead be performed. This transplant consists of removing only the endothelial layer of the patient’s cornea and replacing it with only the endothelial layer of the donor cornea. A DSEK partial-thickness corneal transplant is the treatment of choice for issues affecting the backside of the cornea, such as Fuchs corneal dystrophy. Compared to penetrating keratoplasty, this newer procedure has multiple advantages. It is a shorter surgery, it is a safer surgery, recovery typically takes only 4 months, best vision following recovery does not require the use of a rigid contact lens, and the chances of rejection are much lower. Unfortunately, however, this type of transplant can only be performed in select cases for particular diseases.
For patients with a problem that affects only the endothelial cells, a partial-thickness corneal transplant (or Descemet’s stripping endothelial keratoplasty [DSEK]) can instead be performed. This transplant consists of removing only the endothelial layer of the patient’s cornea and replacing it with only the endothelial layer of the donor cornea. A DSEK partial-thickness corneal transplant is the treatment of choice for issues affecting the backside of the cornea, such as Fuchs corneal dystrophy. Compared to penetrating keratoplasty, this newer procedure has multiple advantages. It is a shorter surgery, it is a safer surgery, recovery typically takes only 4 months, best vision following recovery does not require the use of a rigid contact lens, and the chances of rejection are much lower. Unfortunately, however, this type of transplant can only be performed in select cases for particular diseases.


